Does Antidepressant Discontinuation Affect Psilocybin's Benefits in Depression Treatment?

This is a research paper summary written by Tommaso Barba, a PhD candidate at the Centre for Psychedelic Research at Imperial College London.
Summary
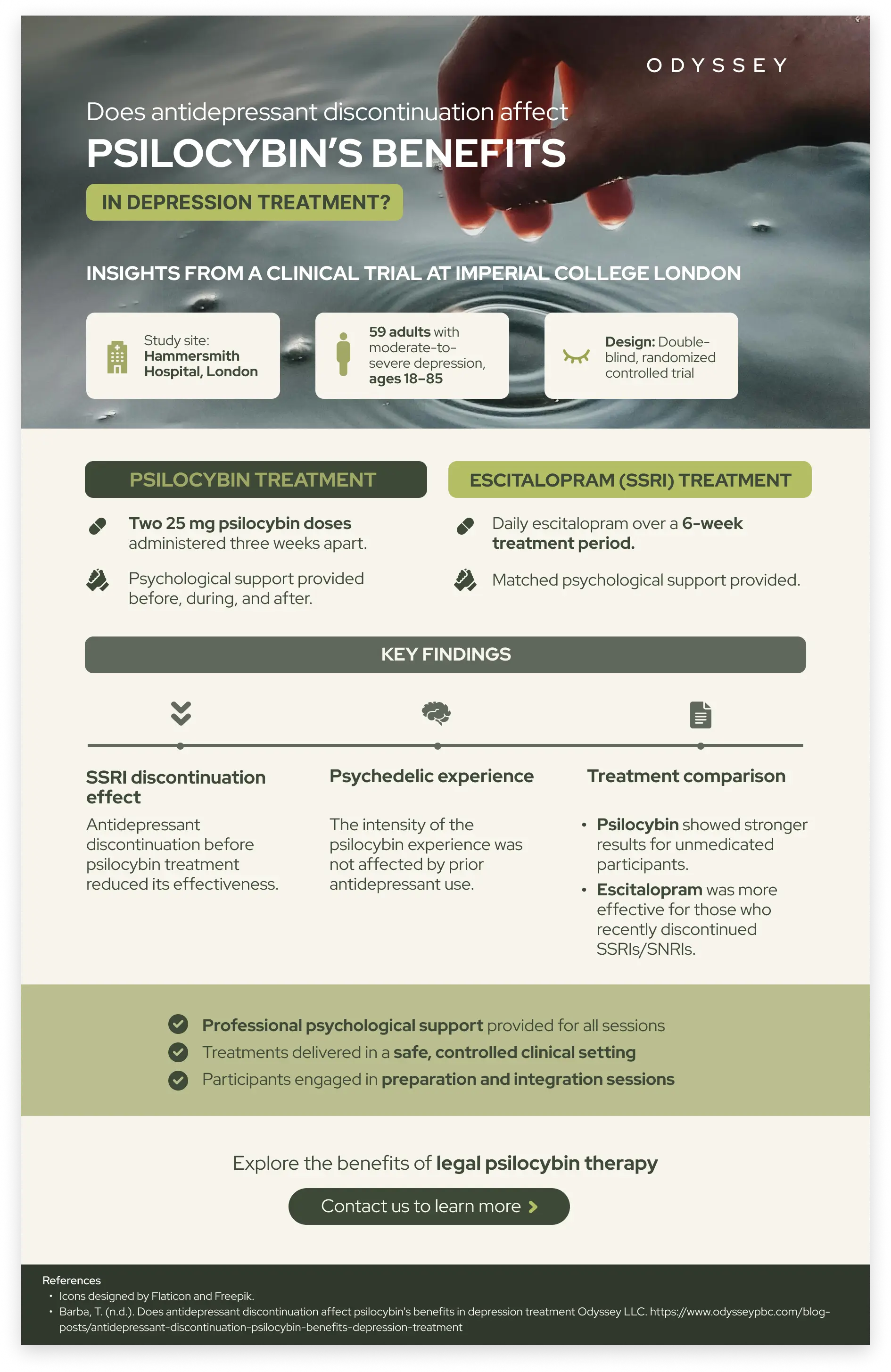
Title: Effects of discontinuation of serotonergic antidepressants prior to psilocybin therapy versus escitalopram for major depression
Objective
The study aimed to investigate the impact of discontinuing serotonergic antidepressants (SSRIs/SNRIs) prior to psilocybin therapy compared to continuing treatment with escitalopram for individuals with major depressive disorder (MDD). Specifically, the research explored how stopping SSRIs/SNRIs might influence psilocybin's effectiveness.
Why were participants withdrawn from antidepressants?
Participants were withdrawn from antidepressants to evaluate whether the absence of ongoing SSRI/SNRI treatment would allow psilocybin to exert its full therapeutic potential without the interference of altered serotonin receptor sensitivity caused by conventional antidepressants. The reason for this was because some previous research (Strassman et al., 1992) showed that SSRI treatment could reduce the psychedelic effects of psilocybin. However, more recent studies have suggested that this might not necessarily be the case (Goodwin et al., 2024), and the true impact remains uncertain.
Details
- The study compared two treatment groups for MDD: one receiving psilocybin and the other receiving escitalopram.
- Psilocybin has been emerging as a potential alternative treatment for depression, particularly for patients who do not respond well to traditional antidepressants. Understanding how previous use of SSRIs/SNRIs impacts psilocybin's efficacy is critical for developing safe and effective treatment protocols.
Number of Participants: A total of 59 participants were enrolled in the study, divided between the two treatment groups to compare the effectiveness of psilocybin versus escitalopram. The relatively small sample size was a limiting factor, but it allowed for a controlled and detailed analysis of each participant's response to the treatment.
Demographics: Participants ranged in age from 18 to 85 years, with both men and women included. All participants had moderate-to-severe major depression.
Study Design: This was a double-blind, randomized controlled trial. Participants received either two doses of psilocybin or a 6-week course of escitalopram, each supplemented with psychological support. The double-blind design ensured that neither the participants nor the researchers knew which treatment was being administered, reducing bias and increasing the reliability of the results. Psychological support included preparatory sessions before dosing and integration sessions afterward to help participants process their experiences and maximize the therapeutic potential of the intervention.
Location: The study was conducted at Hammersmith Hospital in London, Uk and performed by team members of the Centre for Psychedelic Research at Imperial College London.
Dosing:
- Psilocybin Group: Participants received two 25 mg doses of psilocybin, administered three weeks apart. This dosage was chosen based on prior research suggesting its efficacy in reducing depressive symptoms. Each dosing session was accompanied by therapeutic support to help participants navigate the intense experiences associated with psilocybin.
- Escitalopram Group: Participants received two 1 mg doses of psilocybin (as a placebo) and a 6-week course of escitalopram administered daily. The escitalopram group also received psychological support to match the support given to the psilocybin group, ensuring that any differences in outcomes were not due to discrepancies in the level of care provided.
Outcome Measures
The primary outcome was the change in depression severity, assessed using the Quick Inventory of Depression Symptomology Self-Report (QIDS-SR16). Secondary measures included the Beck Depression Inventory (BDI), the Hamilton Depression Rating Scale (HAM-D), and the Warwick-Edinburgh Mental Well-being Scale (WEMWBS). These additional measures provided a comprehensive assessment of participants' mental health, capturing both the severity of depressive symptoms and broader aspects of well-being.
Results/Findings:
- Participants who discontinued SSRIs/SNRIs before the trial showed a reduced treatment effect from psilocybin compared to those who were unmedicated at the start of the trial. This suggests that previous exposure to SSRIs/SNRIs may blunt the therapeutic effects of psilocybin, possibly due to changes in serotonin receptor sensitivity.
- Antidepressant discontinuation did not significantly affect the intensity of the acute psychedelic experience. Participants reported similar subjective experiences during psilocybin sessions regardless of whether they had discontinued antidepressants. This indicates that the acute effects of psilocybin are not directly impacted by recent SSRI/SNRI discontinuation, although the long-term therapeutic benefits might be.
- Psilocybin treatment showed better outcomes than escitalopram on all secondary measures in participants who were unmedicated at the start, while escitalopram was more effective for those who had recently discontinued SSRIs/SNRIs. This suggests that psilocybin may be particularly beneficial for individuals not currently using antidepressant medications, whereas escitalopram may be more suitable for those transitioning from other SSRIs/SNRIs.
Conclusion
Discontinuing SSRIs/SNRIs before psilocybin therapy may reduce treatment response, highlighting the need for careful management during the transition from conventional antidepressants to psychedelic-assisted therapy. The findings suggest that individuals who are tapering off antidepressants may require a longer washout period or alternative tapering strategies to optimize the benefits of psilocybin. Further research is needed to confirm these findings and explore the underlying mechanisms, such as serotonin receptor regulation and individual differences in drug metabolism.
Significance
The findings suggest that stopping SSRIs/SNRIs prior to psilocybin therapy can affect treatment efficacy, emphasizing the importance of careful management of antidepressants for patients receiving psychedelic therapy. A gradual approach to tapering off antidepressants may be necessary to minimize any negative impact on the effectiveness of psilocybin. It is also important to note that these findings contrast with a recent paper on treatment-resistant depression titled "The Impact of Antidepressant Discontinuation Prior to Treatment with Psilocybin for Treatment-Resistant Depression" by Lindsey Marwood et al. (2024). In that study, antidepressant discontinuation was not found to compromise the efficacy of psilocybin treatment. The authors suggested that psilocybin's therapeutic effects and the subjective psychedelic experience were unaffected by recent discontinuation of SSRIs/SNRIs, indicating that stopping antidepressants may not necessarily hinder the success of psilocybin therapy. This discrepancy highlights the need for further research to reconcile these differing findings and clarify the role of antidepressant discontinuation in psychedelic-assisted treatment.
References
- Erritzoe, D., Barba, T., Spriggs, M. J., Rosas, F. E., Nutt, D. J., & Carhart-Harris, R. (2024). Effects of discontinuation of serotonergic antidepressants prior to psilocybin therapy versus escitalopram for major depression. Journal of Psychopharmacology, 38(5), 458-470.
- Goodwin, G. M., Croal, M., Feifel, D., Kelly, J. R., Marwood, L., Mistry, S., O'Keane, V., Peck, S. K., Simmons, H., Sisa, C., Stansfield, S. C., Tsai, J., Williams, S., & Malievskaia, E. (2023). Psilocybin for treatment resistant depression in patients taking a concomitant SSRI medication. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 48(10), 1492–1499.
- Strassman, R. (1992). Human Hallucinogen Interactions with Drugs Affecting Serotonergic. Neuropsychopharmacology, 7(3).
- Marwood, L., Croal, M., Mistry, S., Simmons, H., Tsai, J., Young, M. B., & Goodwin, G. M. (2024). The Impact of Antidepressant Discontinuation Prior to Treatment with Psilocybin for Treatment-Resistant Depression. Journal of Psychiatric Research.
Related articles to read:

.svg)









.svg)