Psilocybin Therapy for Depression

Odyssey Take: Reviewing The Evidence On Psilocybin Therapy For Depression
- The data on psilocybin therapy for Treatment-Resistant Depression is less exciting. Psilocybin for TRD resulted in a clinically significant response in approximately 40% of cases in the weeks following a session, and approximately 25% in the months following. While these results are based primarily on one single-dose study, for those who have struggled with depression for years and tried numerous treatments, it’s important to know that psilocybin may not provide the results they hope for.
- The most interesting finding for us was from a 2021 trial conducted at Johns Hopkins University. Participants received two psilocybin sessions with supportive psychotherapy, and researchers found a rapid decrease in depression scores that continued through follow-ups at 1 month, 3 months, 6 months, and 12 months post-treatment. At 12 months, treatment response rates were an impressive 75%, and remission rates were 58%. While this was a small study of 24 participants, these results are notable as they include a relatively long follow-up period, and suggest that two psilocybin sessions may be more effective than one, especially for lasting benefit.
Written by Aaron Nesmith-Beck & the Odyssey Team
Clinically reviewed by Brian Pilecki, PhD
Evidence is growing for the use of psilocybin-assisted therapy in the treatment of depression, including both major depressive disorder (MDD) and treatment-resistant depression (TRD). In this article, we describe the condition of depression, review the published literature on psilocybin for depression, and discuss potential mechanisms of action. We then provide an overview of the efficacy and benefits, protocol and dosage, and side effects of psilocybin for depression, based on existing research. Finally, we discuss microdosing for depression, provide an overview of ongoing research, and highlight the experience of a former Odyssey client who’s depression substantially improved after their psilocybin session. We aim to provide a balanced overview of current evidence that can serve as a resource for individuals suffering from depression, their loved ones, and their medical or mental health care providers.
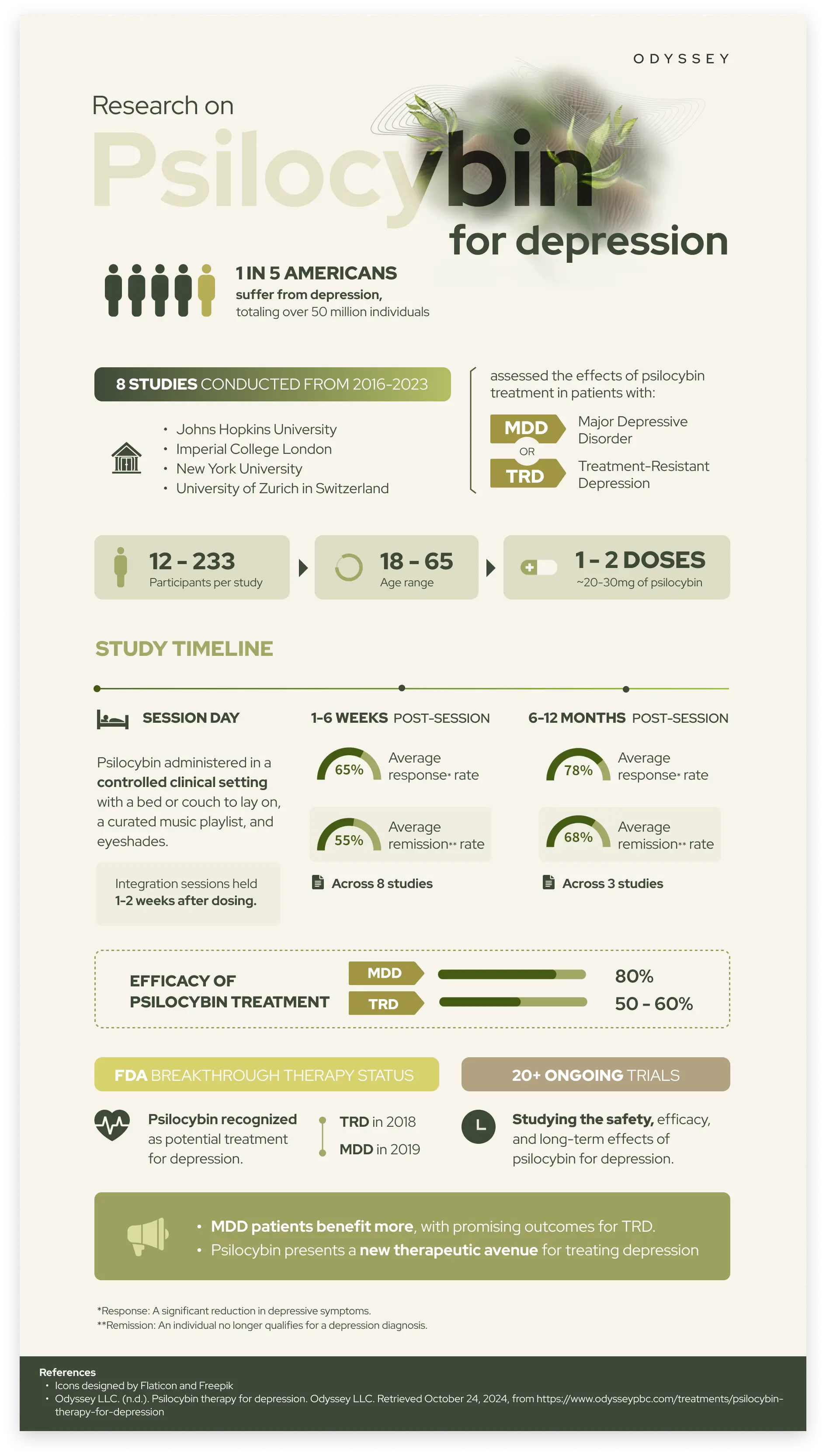
Depression: One of the Largest Mental Health Challenges in Scope and Scale
Depression is a condition characterized by sustained low mood and/or loss of pleasure or interest in usual activities, as well as possible functional impairment.1 Depression is a leading cause of disability worldwide, affecting hundreds of millions of people around the globe.2 Major depressive disorder, the psychiatric diagnosis for depression as defined in the DSM-5, has an estimated lifetime prevalence of 20% in US adults. This means clinical depression affects over 50 million Americans directly, and tens of millions more with its downstream effects.3 Depression impacts quality of life, daily functioning, and overall wellbeing. It is often comorbid with anxiety, substance abuse, and other mental health challenges.4 There is also a significant relationship (often bidirectional comorbidity) between depression and a range of physical diseases.5
Current treatments for depression include psychotherapy and antidepressant prescription medications such as selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs). While these medications can be effective, a majority of patients do not achieve remission.6 Standard antidepressants are also associated with a range of undesirable side effects, a delayed onset of weeks to months, high relapse rates, and withdrawal syndrome.7 Some research suggests antidepressants may be no more effective than placebo, and may not improve patients’ quality of life over longer periods post-treatment.8,9
Considering the widespread impact of depression, and the limited efficacy and potential downsides of existing treatments, there is a significant need for novel treatment methods. Research suggests that psilocybin, especially when administered in a therapeutic setting with professional support, may be an effective treatment for depression.
Published Research Studies on Psilocybin for Depression
The published literature on psilocybin for depression includes controlled trials and proof-of-concept studies from Johns Hopkins, New York University, Imperial College London, and other institutions. Relevant findings from survey studies and population level studies are also included.
A quick note on terminology: you’ll see us refer to rates of “response” and “remission” when discussing trial outcomes. These are standard measurements used to assess treatment effectiveness. “Response” refers to a significant reduction in depressive symptoms, and is generally defined as a 50% or greater reduction in scores on a standardized measure of depression. “Remission” refers to the near or complete absence of any depressive symptoms, meaning that an individual no longer qualifies for a depression diagnosis.
Clinical Trials on Psilocybin for Depression
Psilocybin for Major Depressive Disorder
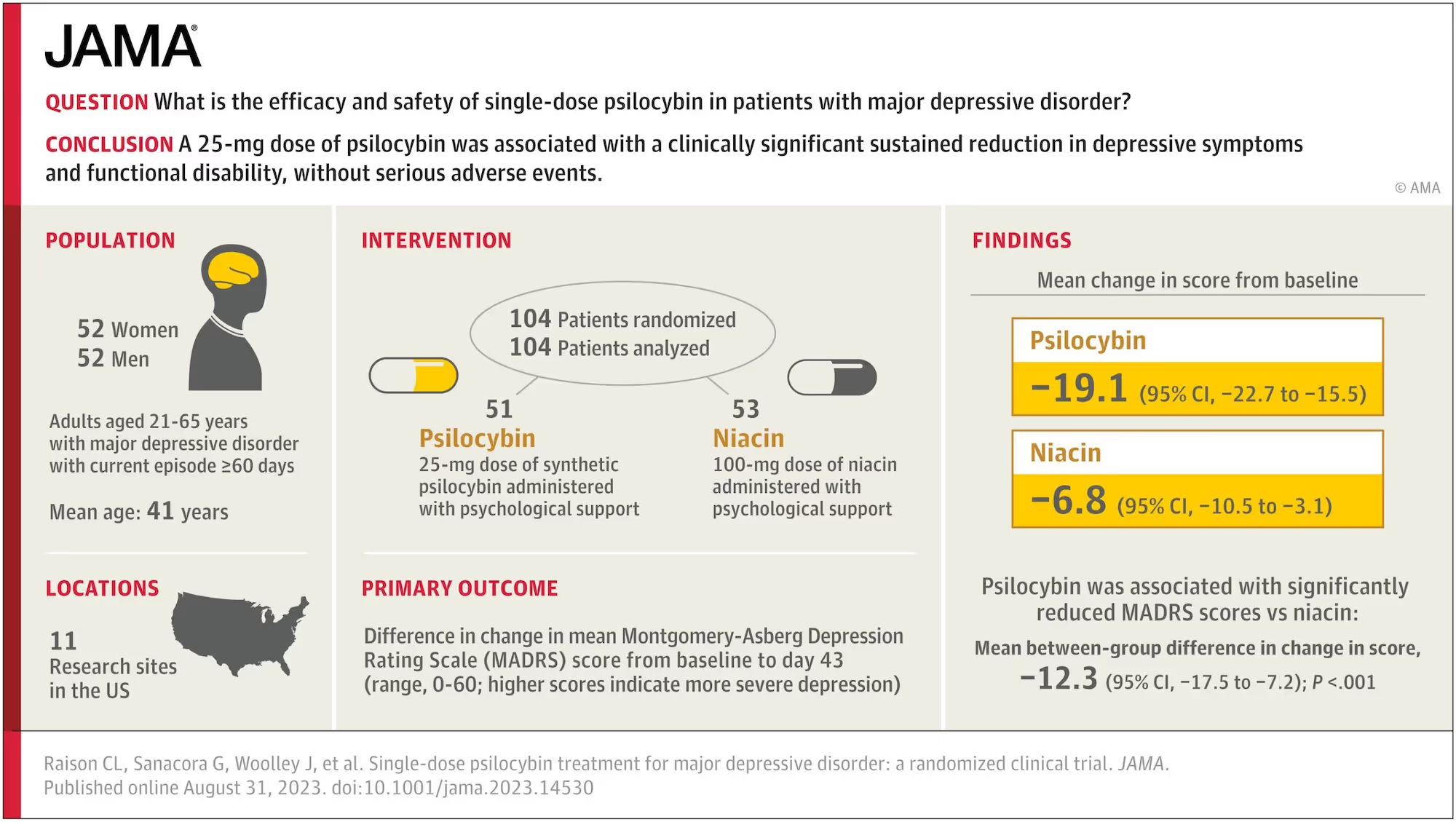
A randomized, placebo-controlled trial was conducted from 2019-2022 at 11 US sites, studying the effects of a single dose of psilocybin with psychological support in 104 patients with major depressive disorder. Findings indicate that psilocybin treatment was associated with a significant reduction in depressive symptoms and functional disability, without serious adverse events. 41.7% of participants who received psilocybin had a sustained response, and 25% a sustained remission, as assessed at day 8, 15, 29, and 43 following the session. Psilocybin treatment was also associated with reduced anxiety, improved quality of life, and did not cause the emotional blunting often seen with conventional antidepressants.10
Odyssey Take: Research on psilocybin for Major Depressive Disorder is promising!
Across six studies, the average response rate in the 1-6 weeks following psilocybin treatment was approximately 65%, and the average remission rate was approximately 55%. Three of these studies measured outcomes over a longer period, and response rates in the 6-12 months following treatment were approximately 78%, and remission rates were approximately 68%. Adverse events were observed in 0-3% of participants the weeks and months following treatment.
Most studies used a single high dose of psilocybin (25mg or higher), one used a single moderate dose (approx. 16mg), and two used two doses. Results indicate that the high dose range (25mg or higher) is most likely to be effective in treating depression, and that two doses may be more effective than one. While these results are encouraging, it’s important to note that research is still early, and most studies have relatively small sample sizes. Below we review the research in more detail.
A 2021 randomized clinical trial conducted at the Center for Psychedelic and Consciousness Research at Johns Hopkins University administered two psilocybin sessions with supportive psychotherapy to 24 participants. Researchers found a rapid decrease in depression score from baseline to the day following the session, and these results remained consistent through a 4-week follow-up period, with no serious adverse events. 71% of participants had a clinically significant response at weeks 1 and 4 following the treatment. 58% of participants were in remission at week 1, and 54% at week 4.11
Participants in this study also completed follow-up assessments in the 12 months following their treatment. Large decreases in depressive symptoms were observed at 1 month, 3 month, 6 month, and 12 month follow-up. At 12 months, treatment response rates were 75% and remission rates were 58%. No serious adverse events related to psilocybin were observed in the follow-up period, and no participants reported psilocybin use outside of the context of the study.12
A 2023 placebo-controlled, double-blind, randomized clinical trial conducted at the University of Zurich in Switzerland studied the effects of psilocybin on 52 participants diagnosed with major depressive disorder. Participants received either a single moderate dose of psilocybin, or a placebo, with psychological support, and were assessed for depressive symptoms up to 14 days following the session. Participants who received psilocybin showed significant improvements in depressive symptoms compared to the placebo group, and 54% met criteria for remission at the 14 day mark. No serious adverse events were observed.13
A 2021 double-blind, randomized, controlled trial conducted at Imperial College London compared the effects of psilocybin and escitalopram, a common antidepressant, on 59 patients with depression. Patients received either two doses of psilocybin, spaced 3 weeks apart, or daily escitalopram for 6 weeks. The psilocybin group showed 70% response and 57% remission rates, compared to 48% and 28% for the escitalopram group, respectively. This difference was deemed not to be clinically significant. Psilocybin outperformed escitalopram on secondary measures, including three additional common measures for depression, participant ratings of wellbeing, and reductions in suicidal ideation, trait anxiety, experiential avoidance, and others.14
Two 2016 studies, one at Johns Hopkins University and one at NYU, investigated psilocybin's effects on cancer patients with end-of-life anxiety and depression. They found response rates of approximately 70-80% and remission rates of approximately 65-80%, that were sustained at 6-month follow-up. Other benefits including increases in measures of quality of life, wellbeing, life meaning, optimism, and spiritual significance were attributed to the psilocybin experience.15,16
Psilocybin for Treatment-Resistant Depression
Odyssey Take: Research on psilocybin for Treatment - Resistant Depression is less promising.
The initial research results on psilocybin for Treatment-Resistant Depression have been less encouraging. Across two studies, the average response rate in the 1-3 weeks following psilocybin treatment was approximately 40%, and the average remission rate was approximately 32%. At 3 months following treatment, the average response rate was approximately 25%. One small study found response and remission rates of 58% and 42% at 3 months, respectively, but a much larger study found no significant difference in response rates compared to placebo. Severe adverse events were observed in 3-9% of participants in the weeks and months following treatment.
Across these two studies, a high dose (25mg), moderate dose (10mg), and placebo dose (1mg) of psilocybin was used. Results indicate that the high dose range is most likely to be effective in treating TRD, and that a moderate dose is not likely to be effective.
Overall, we’re less excited about the potential of psilocybin for TRD, based on current evidence. While research results are somewhat disappointing, it’s important to note that most of the data comes from a single clinical trial that used a single dose of psilocybin, capped at 25mg. This trial also employed “psychological support” rather than “psychotherapy” alongside psilocybin treatment, which may suggest a less intensive overall treatment approach. We’re curious about the potential of higher doses and/or multiple dosing sessions with psychotherapy as support in future research. Below we review the published studies in more detail.
A 2022 study tested a proprietary, synthetic formulation of psilocybin in 233 participants with treatment-resistant depression. Participants had a current episode of depression that had not responded to two to four prior forms of treatment, making psilocybin a third, fourth, or fifth-line treatment. Participants received a single dose of either 25 mg, 10 mg, or 1 mg (intended as placebo) of psilocybin, with psychological support before, during, and after the session.
At 3 weeks post-treatment, response rates were 37% in the 25 mg group, 19% in the 10 mg group, and 18% in the 1 mg group. Remission rates were 29% in the 25 mg group, 9% in the 10 mg group, and 8% in the 1 mg group. At 12 weeks, there was no significant difference in reported depression symptoms between the groups.17 Improved disability scores, general functioning, quality of life, and cognitive function were observed in a dose-dependent manner: strongest for the 25 mg group, less strong for the 10 mg group, and weakest for the 1 mg group.18
In the weeks and months following the session, severe adverse events were reported by approximately 3-9% of participants in the 25mg and 10mg groups. These events included suicidal ideation, suicidal behavior, intentional self-injury, and hospitalization (for severe depression).17 The extent to which these adverse events are attributable to psilocybin’s effects, as opposed to the inherently higher risk associated with a TRD population, is unclear.
A 2016 open-label feasibility study conducted at Imperial College London assessed the safety and efficacy of psilocybin for TRD in 12 patients. Patients received two doses of psilocybin, first a 10 mg safety dose and then a 25 mg treatment dose, spaced one week apart. The response rate was 67% and remission rate was 58% one week after treatment. At three months post-treatment, 58% of patients maintained their response and 42% remained in remission. No serious adverse events were observed. The study authors note caution around interpreting these results, as small studies typically have inflated effect sizes, and 5 of the 12 patients showed a degree of relapse at 3 months.19
Survey Studies Assessing Psilocybin and Depression
The Center for Psychedelic and Consciousness Research at Johns Hopkins University conducted a survey study assessing the impact of psilocybin on mental health in individuals who consumed psilocybin naturalistically (outside of a research setting). 2,833 respondents completed assessments before psilocybin use, 1,182 completed the 2–4 week post-use survey, and 657 completed the final follow-up survey 2–3 months after psilocybin use.
According to the findings, psilocybin mushroom use was associated with significant improvements in mental health, wellbeing, and psychological functioning. Persisting reductions in depression were found, with a moderately large effect size. While most reported effects were positive, around 9% of participants reported enduring difficulties following their experience, the most common of which were mood fluctuations and depressive notions.20 This is consistent with other findings that while psilocybin seems to result in mostly or entirely positive outcomes for most people, in a minority of cases there can be lasting adverse effects.21
Population Studies: Psilocybin Associated with Improved Mental Health
Several studies have examined the relationship between psychedelic use and mental health at the population level. While these studies do not directly assess psilocybin's effects on depression, they provide another form of evidence based on much larger datasets than any controlled trial.
A study using data from over 100,000 US adults found no associations between lifetime psychedelic use and increased rates of mental illness, and a similar study of over 20,000 US adults found that psychedelics were not linked to mental health problems or suicidal behavior.22,23
A 2015 study of over 190,000 US adults found that lifetime classic psychedelic use (psilocybin, LSD, or mescaline) was associated with “a 19% reduced likelihood of past month psychological distress, a 14% reduced likelihood of past year suicidal thinking, a 29% reduced likelihood of past year suicidal planning, and a 36% reduced likelihood of past year suicide attempt”.24 Since depression and suicidality are closely linked, this finding supports the notion that psilocybin can be helpful for those with depression.
Mechanisms of Action: How Might Psilocybin for Depression Work?
Psilocybin’s mechanisms of action for the treatment of depression have been studied at multiple levels of analysis. Most of the recent research on psilocybin for depression has been focused on outcome—essentially, to what degree did psilocybin-assisted therapy work. Much less is known about underlying mechanisms of action. In other words, we still cannot say how it works. However, initial evidence suggests several potential processes relevant to therapeutic change. Here we provide an overview of each, followed by discussion.
Acute Biological Effects
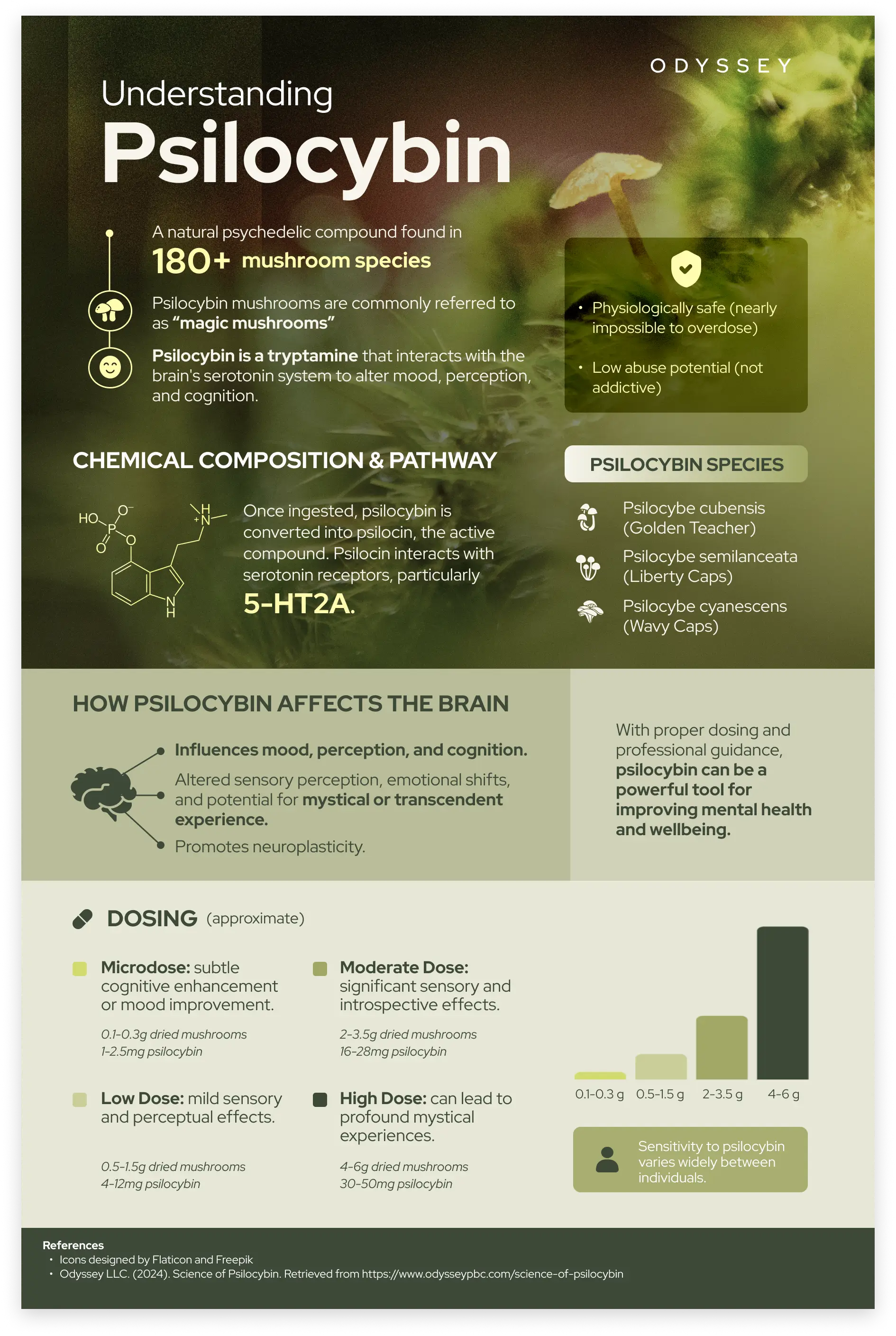
In general, psilocybin exerts its psychological effects primarily through serotonergic pathways in the brain and body. Once ingested, psilocybin is converted to psilocin, which then binds to serotonin receptors, in particular acting as an agonist at the 5-HT2a receptor.25 Serotonin receptors are abundant in brain regions such as the prefrontal cortex, which is involved in mood, cognition, and perception, and relevant to depression.
Psilocybin also affects glutamate, an excitatory neurotransmitter and the most abundant neurotransmitter in the brain, and dopamine, which plays a key role in reward, motivation, and pleasure. Enhanced glutamate signaling and increased dopamine release may also contribute to psilocybin’s antidepressant effects.26,27
Changes in brain network activity and connectivity
At the brain network or functional connectivity level, psilocybin has been shown to alter connectivity within and between brain regions. It impacts regions that include the amygdala, prefrontal cortex, and hippocampus.28
A particularly relevant area is the default mode network (DMN), which is highly involved in self-referential mental activity (e.g. thoughts about one’s personality, recalling past personal experiences, envisioning future personal events, etc.). The DMN is often overactive in individuals with depression, and this can manifest as rumination, self-criticism, or persistent negative thoughts.29 It is hypothesized that by changing activity in the DMN, psilocybin reduces this overactivity, leading to a decrease in depressive symptoms. While the DMN has received much attention for explaining how psilocybin works, research is still preliminary and there are likely many other networks yet to be studied that are relevant to psilocybin’s impact on the brain.
Psilocybin increases flexibility in other brain networks, including the executive network (EN) and salience network (SN).30 The EN and SN are associated with cognitive flexibility and attention switching, and impaired functioning of these networks has been reported in depression. Increased flexibility in these regions following psilocybin may be an important part of its therapeutic mechanism of action.31
Psilocybin also affects activity in the amygdala, which is hyperactive in many individuals with depression. A hyperactive amygdala contributes to heightened emotional responses, especially to negative stimuli. A study from Imperial College London suggests that psilocybin’s effects on the amygdala relate to an increase in emotional sensitivity and acceptance after psilocybin.32
Psychological and emotional effects of the psilocybin experience
At the psychological and emotional level, psilocybin’s subjective effects likely play a role in the alleviation of depression. In general, psilocybin helps process psychological and emotional material, and creates new perspectives, insights, and ways of relating to familiar internal and external phenomena.
Multiple studies have shown that psilocybin’s ability to increase psychological flexibility is an important aspect of its effects on depression.33,34,35 Psilocybin has also been shown to reduce rumination and thought suppression (deliberate and effortful attempts to avoid distressing thoughts or memories), which are characteristic of depression.36
Psilocybin can help create a shift from avoidance to acceptance of emotions, resulting in improved mental health. During the course of working with psilocybin, new and helpful ways of relating to emotion may be uncovered naturally during a session and/or learned from facilitators during preparation and integration. Two patients from an Imperial College London study describe their experience:
“There was a lot of sadness, really really deep sadness: the loss the grief, it was love and sadness together, and letting go, I could feel the grief and then let it go because holding onto it was hurting me, holding me back. It was a process of unblocking.”
“I saw negative patterns in my life where if something bad happens, I used to just put it [to the back of my mind]. Afterwards, I allowed myself to experience everything - even if it is sadness. Now I know how to deal with my feelings rather than repress them.”
The same study also found that psilocybin increased connectedness to self, others, and the world. Patients describe their experience:
“I had an encounter with a being, with a strong feeling that that was myself, telling me it’s alright, I don’t need to be sorry for all the things I’ve done. I had an experience of tenderness towards myself. During that experience, there was a feeling of true compassion I had never felt before.”
“I got a wider perspective, I stepped back. It helped me appreciate that the world is a big place that there’s a lot more going on than just the minor things that were going on in my head.”
“[During the dose] I was everybody, unity, one life with 6 billion faces, I was the one asking for love and giving love, I was swimming in the sea, and the sea was me.”37
The mystical or spiritual aspects of the psilocybin experience also seem to play a key role in its treatment of depression.38,34 This involves, but is not synonymous with, the phenomenon of loss of the ordinary sense of self or “ego dissolution”. A mystical-type experience may include a sense of awe, cosmic unity, acutely experienced bliss or boundlessness, the experience of contacting a reality that is “more real” or “more true” than ordinary reality, and an experience of direct connection with the divine. Along with treating depression, these experiences have been shown in research to result in decreased stress and anxiety, reductions in addictive behavior, improved overall wellbeing, and a range of other benefits.39
Therapeutic alliance between facilitator and participant
The therapeutic alliance—broadly defined as the sense of collaboration between facilitator and participant or client—has shown to be instrumental in positive outcomes for psilocybin therapy for depression.
A 2024 study assessed the therapeutic alliance between study participants and facilitators in a 2021 clinical trial conducted at Johns Hopkins University. Overall, a stronger therapeutic alliance (as assessed at the final integration session) predicted improvements in depression at 4 weeks, 6 months, and 12 months post-session. A stronger therapeutic alliance was also correlated with higher ratings of mystical experience and psychological insight, which both correlated with improvements in depression.40
A 2021 study analyzed therapeutic alliance in a 2021 Imperial College London study comparing psilocybin and escitalopram for depression. Researchers found that a stronger therapeutic alliance predicted greater emotional breakthrough and mystical experience during sessions, and greater improvements in depression scores 3 weeks after the second psilocybin session.41
Discussion: Psilocybin’s mechanisms of action compared to standard antidepressants
Psilocybin and standard antidepressants such as SSRIs, SNRIs, and others primarily act on the serotonin system. However, the mechanisms of action for therapeutic change seem quite different, especially at the experiential level. Standard antidepressants often produce an emotional blunting effect, reducing negative emotion and depressive symptoms, but in doing so reducing the intensity of all emotion.42,43
Psilocybin, by contrast, allows individuals to engage more fully with their emotions, leading to greater acceptance and decreased emotional avoidance.38 In the study comparing psilocybin to escitalopram, researchers found that psilocybin reduced thought suppression, while escitalopram did not.36
Another analysis found that patients had increased emotional responsiveness to images of happy and fearful faces after psilocybin, which did not occur with escitalopram. Participants in this study described the contrast between the experience of psilocybin and previous treatments, which they felt reinforced emotional avoidance and disconnection.44
Discussion: What explains higher rates of adverse events in patients with TRD compared to MDD?
Higher rates of adverse events following psilocybin treatment have been observed in patients with treatment-resistant depression (TRD) compared to those with major depressive disorder (MDD). Given that TRD is inherently a higher-risk and more severe condition, higher baseline rates of adverse events are to some extent expected.
If psilocybin brings repressed or unprocessed psychological and emotional material into one’s awareness, this may also contribute to the higher rates of adverse events in patients with TRD.45 TRD patients may have more (in amount and/or severity) of this material, which underlies their persistent and entrenched depression. When this material is uncovered during a psilocybin experience, it may be distressing or destabilizing.
TRD patients may therefore require additional support, in the form of additional psilocybin sessions, additional integration sessions, or specific types of psychotherapy. While a supportive context is crucial for all therapeutic psilocybin work, it may be especially important for individuals with TRD. This is just one hypothesis, and more research is needed.
Efficacy and Benefits of Psilocybin for Depression
In studies on psilocybin for major depression, on average, in the 2-6 week period following a psilocybin session, response rates were approximately 67% and remission rates were approximately 49%. In the 6-12 months following a session, response rates were approximately 77% and remission rates were approximately 69%.
In studies on psilocybin for treatment-resistant depression, in the 1-3 weeks following the session, response rates were approximately 40% and remission rates were approximately 32%. At 3 months, response rates were approximately 25%, and one study of 12 participants found a 42% remission rate at 3 months.
Among the populations studied for psilocybin's effects on depression, end-of-life cancer patients have shown the highest rates of response and remission, followed by individuals with MDD, and then individuals with TRD. While these response and remission rates are impressive, it’s important to note that most studies to date have relatively small sample sizes, and more research is needed to draw definite conclusions about psilocybin’s efficacy.
Along with the alleviation of depressive symptoms, psilocybin can confer a range of benefits. As discussed, psilocybin creates new perspectives, insights, and ways of relating to familiar internal and external phenomena. It helps process psychological and emotional material, and increases acceptance of emotions. It can bring about a greater sense of connection to ourselves, to others, and to the world. General increases in wellbeing, quality of life, and spiritual meaning and significance are often reported.
Patient’s accounts of their experience are instructive:
“I was thinking about relationships I had with other people and thinking I could see them clearly almost as if for the first time. I had fresh insight into things. It was almost as if suddenly the scales dropped from my eyes, I could see things as they really are.”
“[After the dose] When I went outside, everything was very bright and colourful and it felt different. I noticed things I didn’t notice usually, the leaves on the trees and the birds, small details.”
After psilocybin, some describe a kind of “reset”:
“It was a change of state, to be stuck in that place of rumination and to be able to move out. It reconfigures you somehow.”
“The reset switch had been pressed so everything could run properly, thoughts could run more freely, all these networks could work again. It unlocked certain parts which were restricted before.”37
Psilocybin Protocol and Dosage for Depression
Studies on psilocybin for major depression typically use one or two doses of synthetic psilocybin, most often in the high range of approximately 25-35 mg of psilocybin, though one study used a moderate dose of approximately 16 mg. When two doses are administered, they are spaced approximately 1.6 or 3 weeks apart. For treatment-resistant depression, studies have generally used one moderate dose (10 mg) and/or one high dose (25 mg) of synthetic psilocybin, with participants who took both doses doing so 1 week apart. A protocol involving a single dose or two doses of psilocybin may offer a substantial advantage over standard antidepressants, which typically require daily administration.
Overall, evidence suggests that a high dose of psilocybin (approximately 25 mg or higher) is likely to be most effective in treating depression. A moderate dose (approximately 10-20 mg) may be effective for major depression, but is unlikely to be effective for treatment-resistant depression. This aligns with the understanding that therapeutic effect is linked to the intensity of the subjective psychedelic experience, which is generally dose-dependent. Two doses may be more effective than one, although this is less clear.
The high dose range is consistent with that used in most modern psychedelic clinical trials and research studies, and the dose range we use at Odyssey. We typically start with a 25mg dose, and often increase as needed. Oregon regulations allow for a maximum dose of up to 50mg, which provides flexibility in the case that an individual requires a substantially higher dose (for example, if they are taking a prescription medication that blunts psilocybin’s effects). While synthetic psilocybin is used in research studies, organic psilocybin is used in Oregon. Whether there is any meaningful difference between the two is currently unknown.
All studies include therapeutic support from facilitators before, during, and after a session. Sometimes, this support is referred to as 'psychotherapy,' and other times as 'psychological support.' Unfortunately, the details of the therapeutic support in psychedelic studies is often not well defined, making it difficult to compare approaches.46 The session protocol involves laying down, wearing eyeshades, and listening to a curated playlist while focusing inward with an attitude of openness and acceptance. This matches the protocol we use at Odyssey, which is grounded in science and evidence.
Side Effects of Psilocybin for Depression
Psilocybin is generally safe and well-tolerated, especially when administered in a controlled setting with professional support.47 It can moderately increase heart rate and blood pressure, but even at high doses, this effect is mild.48
One of the most commonly reported side effects of psilocybin is nausea during the experience. This can sometimes be alleviated by consuming ginger, such as ginger capsules or ginger tea. Post-experience headaches are another common side effect, and can be mitigated by over-the-counter pain medication.49 Psilocybin can also cause body shaking or trembling, which some individuals may find unpleasant. In research, side effects reported during and up to 24 hours after sessions are generally limited to nausea and headaches.
Depending on the study, between 0-4% of patients with MDD experienced post-session adverse events, which occasionally required additional psychological or psychiatric support. Among patients with TRD, 3-9% experienced post-session adverse events, including suicidal ideation, intentional self-injury, and hospitalization for severe depression. Overall, the potential for side effects with psilocybin is favorable compared to standard antidepressants, which are often associated with weight gain, sexual dysfunction, emotional blunting, and more.
For more details, see our article on the safety of psilocybin therapy.
Microdosing Psilocybin for Depression
Odyssey Take: It’s unclear if microdosing helps with depression.
Self-reported and observational data shows mental health benefits from microdosing, but the placebo effect may play a role. We’re more excited about high-dose psilocybin in a therapeutic setting with professional support for treating depression, compared to microdosing. Below we review the research in more detail.
One study followed over 900 microdosers for approximately 30 days and found improvements in mood, including reductions in symptoms of depression. This change was most notable in respondents with mental health concerns at the beginning of the study.50
Another study observed positive changes in wellbeing, including improvements in depression, over 4 weeks of microdosing. For participants who were more depressed at the start, this effect occurred within the first week of microdosing. However, researchers also noted that positive expectations predicted of improvements in mental health, suggesting expectations may influence the observed effects.51
Another study found that expectations played a role in microdosing’s effects, but the changes microdosing induced were not the ones people expected, suggesting a complex relationship between expectation and outcome.52 Several other studies have found reported reductions in depression attributed to microdosing.53,54,55
Two controlled studies found no positive impact of microdosing on mental health, however, participants in these studies were considered “mentally healthy” and did not have depression at the beginning of the study.56,57
Microdosing psychedelics, including psilocybin, may pose potential cardiac risks primarily due to their agonist activity on the 5-HT2B receptors, which has been associated with valvular heart disease.58 Although the risk appears to be low at microdoses, the long-term effects remain uncertain, and further research is needed to fully understand the safety profile of microdosing.
Overall, while microdosing may provide benefits for depression for some individuals, the evidence is largely based on self-report and observational analysis. Expectations likely play a role, but the extent and nature of this effect are unclear. The evidence supporting depression treatment with high-dose psilocybin in a therapeutic setting with professional support is substantially stronger than the evidence for microdosing.
Ongoing Research Studies on Psilocybin for Depression
A range of ongoing studies worldwide are investigating psilocybin for depression. We highlight three US-based studies below. For a comprehensive list of ongoing trials, visit clinicaltrials.gov.
Psilocybin for Major Depressive Disorder (MDD)
This phase 3, randomized, double-blind trial conducted by the Usona Institute will evaluate the efficacy, safety, and tolerability of psilocybin in approximately 240 adults with major depressive disorder (MDD) at multiple locations in the United States. Participants will receive either high dose psilocybin (25 mg), low dose psilocybin (5 mg), or inactive placebo, along with preparation and integration support. Trial outcome measures will assess depressive symptoms, functional disability, health-related quality of life, and more, and outcome measures will be taken for up to one year following the session.
Low-Income Group Psilocybin Assisted Therapy for Depression (LIGPATD)
This study in Portland, Oregon plans to investigate the efficacy of a group therapy model in adults in Oregon with a diagnosis of major depression and an income at or below 200% of the federal poverty level. In groups of five to six, participants will undergo a treatment protocol of two group preparation sessions, two psilocybin sessions, and two group integration sessions. Follow-up measures will be taken three months after treatment.
Psilocybin-Assisted Therapy in Treatment-Resistant Depression
A clinical trial at the University of North Carolina, Chapel Hill Medical Center will assess the degree and duration of the effects of psilocybin in individuals with treatment-resistant depression. The study will also compare the effects of one compared to two doses of psilocybin, and follow-up measures will be taken up to 12 months after treatment.
Laura: An Odyssey Psilocybin for Depression Success Story
Laura is a former Odyssey client who was struggling with depression, and experienced substantial benefit following her psilocybin session. Here’s Laura’s experience, in her own words:
“I recently embarked on a guided psilocybin journey, seeking deeper self-understanding and emotional healing. This experience, while challenging, was also imbued with a sense of peace that I had never known. Psilocybin is not for the faint of heart, and the initial phase of my journey was a testament to that. Letting go and allowing the medicine to work its magic was a struggle at first, as I confronted deep-seated issues with relinquishing control.
As the journey progressed, I found myself immersed in a kaleidoscope of vibrant colors and intricate shapes, a sensory overload that was almost overwhelming. This tumultuous phase gradually gave way to a series of transitions, each 'phase' distinct yet interconnected, spanning the six-hour experience. The culmination was a state of absolute bliss, a serene calmness that enveloped me in a way I've never felt in my almost 50 years of existence. I experienced an intense feeling of love, a deep connection with my loved ones, and a profound oneness with the world around me.
Post-journey, my emotional landscape has shifted dramatically. I find myself more in touch with my emotions, often moved to tears not by sadness, but by an overwhelming sense of happiness and gratitude. This heightened emotional awareness has brought a sense of lightness, a pervasive happiness that colors my daily life.
Reflecting on this journey, I can confidently say it has been a pivotal turning point in my life. For me, the experience was like being given a new lens through which to view the world. It's not just a shift in perception; it's an awakening to new dimensions of thought and emotion. I now see the world with a fresh perspective, as if my eyes have been reopened and my heart expanded. This journey has deepened my capacity for love and connection in ways I never thought possible. It's as if I've stepped into a more vivid, more connected version of reality, and the richness of this new perspective is something that transcends traditional value metrics.”
Laura also highlighted the importance of a trusted relationship with her facilitator:
“What I've come to realize is the immense importance of intention and setting. It's crucial to have a clear understanding of what you're seeking to achieve and to choose a facilitator with whom you feel a sense of trust and comfort, especially when it comes to being vulnerable.
My experience with my Odyssey facilitator was nothing short of extraordinary. From the outset, he demonstrated a remarkable ability to connect on a deep, personal level. He took the time to truly get to know me, asking insightful questions that helped him understand my unique background and the specific intentions I had for my journey. His approach wasn't just professional; it was personalized and empathetic.
My facilitator's sensitivity and understanding were especially crucial for me, as someone who has endured childhood trauma. He communicated expectations clearly and worked tirelessly to ensure I felt comfortable and safe throughout the process. His ability to create a trusting environment was instrumental in allowing me to fully engage in the journey."
Laura’s experience reflects many of the research findings we’ve discussed in this article: psilocybin’s facilitation of emotional acceptance, the unitive aspects of the experience, and the increased connectedness to self, others, and the world during and after the session. Her experience also underscores the importance of the therapeutic alliance, which research has shown to be instrumental towards positive outcomes.
While the evidence is promising, it’s important to note that research is still early, and that it’s not possible to guarantee any specific experience of outcome from a psilocybin session. Odyssey does not claim or attempt to treat any medical or mental health condition, and Odyssey services are not a substitute for medical or mental health treatment.

Conclusion
Psilocybin may be a novel and effective treatment for both major depressive disorder (MDD) and treatment-resistant depression (TRD). Given the widespread nature of depression, and the limitations of existing treatments including their efficacy and side effects, new treatment options are needed.
Clinical trials on psilocybin for depression have shown promising results, with relatively high response and remission rates in the weeks and months following treatment. Patients with MDD typically show greater improvement and experience fewer adverse events compared to those with TRD.
A survey study involving 600-1200 individuals showed reductions in depression following naturalistic psilocybin use, lasting up to 2-4 weeks. Population level studies, drawing on data from tens of thousands of people, also support the potential benefits of psilocybin for depression.
Psilocybin’s mechanisms of action in treating depression operate on multiple levels. It primarily affects serotonin receptors in the brain, as well as glutamate and dopamine. Psilocybin alters functional connectivity within and between brain regions, especially the default mode network (DMN), which is heavily implicated in self-referential mental activity.
Psilocybin increases psychological flexibility, emotional acceptance, and connection to self, others, and the world, as well as reducing rumination and thought suppression. Psilocybin can induce a spiritual or mystical-type experience associated with a range therapeutic benefits, including alleviating depression. The therapeutic alliance between a session facilitator and participant has also been shown to be crucial for positive outcomes in psilocybin therapy.
Psilocybin’s ability to surface previously suppressed psychological and emotional material contrasts with the effects of standard antidepressants, which often cause emotional blunting. This effect may partially explain why TRD patients have higher rates of adverse events following psilocybin treatment compared to MDD patients.
Based on current evidence, psilocybin for major depression resulted in a clinically significant response in approximately 70% of cases in the weeks and months following a session. Psilocybin for treatment-resistant depression resulted in a clinically significant response in approximately 40% of cases in the weeks following a session, and approximately 25% in the months following. In addition to alleviating depressive symptoms, psilocybin is associated with increased well-being, quality of life, spiritual meaning, significance, and greater emotional connection and acceptance.
High doses of psilocybin (25 mg or higher) are generally used in the treatment of depression, with research indicating that this dose range is likely to be most effective. Most studies use one dose, with some employing two doses, which may be somewhat more effective for both MDD and TRD.
Side effects during and up to 24 hours after psilocybin sessions are generally limited to nausea and headaches. Adverse events following sessions are uncommon, occurring more frequently in TRD patients (3-9%) than in MDD patients (0-4%).
Microdosing psilocybin may have an effect on depression, but the evidence is inconclusive and primarily based on self-report and observational studies. The evidence base for microdosing for depression is substantially weaker than for high-dose psilocybin administered in a therapeutic setting.
There are a number of ongoing studies on psilocybin for depression in the US and globally. These include a large, multi-site trial, comparisons of high-dose versus low-dose psilocybin, and an analysis of group psilocybin therapy.
We’re grateful to have been able to support Laura, and hope to support many more like her. If you or someone you know is suffering from depression and you’re interested in psilocybin, we invite you to get in touch using the “Start Journey” button at the top of the page. We’d love to connect with you and see if Odyssey’s services are a good fit.
References
1. National Institute of Mental Health. (2024). Depression. U.S. Department of Health and Human Services. Retrieved from https://www.nimh.nih.gov/health/publications/depression
2. Ferrari, A. J., Charlson, F. J., Norman, R. E., Patten, S. B., Freedman, G., Murray, C. J., Vos, T., & Whiteford, H. A. (2013). Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS medicine, 10(11), e1001547. https://doi.org/10.1371/journal.pmed.1001547
3. Hasin, D. S., Sarvet, A. L., Meyers, J. L., Saha, T. D., Ruan, W. J., Stohl, M., & Grant, B. F. (2018). Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA psychiatry, 75(4), 336–346. https://doi.org/10.1001/jamapsychiatry.2017.4602
4. Thaipisuttikul, P., Ittasakul, P., Waleeprakhon, P., Wisajun, P., & Jullagate, S. (2014). Psychiatric comorbidities in patients with major depressive disorder. Neuropsychiatric disease and treatment, 10, 2097–2103. https://doi.org/10.2147/NDT.S72026
5. Berk, M., Köhler-Forsberg, O., Turner, M., Penninx, B. W. J. H., Wrobel, A., Firth, J., Loughman, A., Reavley, N. J., McGrath, J. J., Momen, N. C., Plana-Ripoll, O., O'Neil, A., Siskind, D., Williams, L. J., Carvalho, A. F., Schmaal, L., Walker, A. J., Dean, O., Walder, K., Berk, L., … Marx, W. (2023). Comorbidity between major depressive disorder and physical diseases: a comprehensive review of epidemiology, mechanisms and management. World psychiatry : official journal of the World Psychiatric Association (WPA), 22(3), 366–387. https://doi.org/10.1002/wps.21110
6. Munkholm, K., Paludan-Müller, A. S., & Boesen, K. (2019). Considering the methodological limitations in the evidence base of antidepressants for depression: a reanalysis of a network meta-analysis. BMJ open, 9(6), e024886. https://doi.org/10.1136/bmjopen-2018-024886
7. Gastaldon, C., Schoretsanitis, G., Arzenton, E., Raschi, E., Papola, D., Ostuzzi, G., Moretti, U., Seifritz, E., Kane, J. M., Trifirò, G., & Barbui, C. (2022). Withdrawal Syndrome Following Discontinuation of 28 Antidepressants: Pharmacovigilance Analysis of 31,688 Reports from the WHO Spontaneous Reporting Database. Drug safety, 45(12), 1539–1549. https://doi.org/10.1007/s40264-022-01246-4
8. Munkholm, K., Paludan-Müller, A. S., & Boesen, K. (2019). Considering the methodological limitations in the evidence base of antidepressants for depression: a reanalysis of a network meta-analysis. BMJ open, 9(6), e024886. https://doi.org/10.1136/bmjopen-2018-024886
9. Almohammed, O. A., Alsalem, A. A., Almangour, A. A., Alotaibi, L. H., Al Yami, M. S., & Lai, L. (2022). Antidepressants and health-related quality of life (HRQoL) for patients with depression: Analysis of the medical expenditure panel survey from the United States. PloS one, 17(4), e0265928. https://doi.org/10.1371/journal.pone.0265928
10. Raison, C. L., Sanacora, G., Woolley, J., Heinzerling, K., Dunlop, B. W., Brown, R. T., Kakar, R., Hassman, M., Trivedi, R. P., Robison, R., Gukasyan, N., Nayak, S. M., Hu, X., O'Donnell, K. C., Kelmendi, B., Sloshower, J., Penn, A. D., Bradley, E., Kelly, D. F., Mletzko, T., … Griffiths, R. R. (2023). Single-Dose Psilocybin Treatment for Major Depressive Disorder: A Randomized Clinical Trial. JAMA, 330(9), 843–853. https://doi.org/10.1001/jama.2023.14530
11. Davis, A. K., Barrett, F. S., May, D. G., Cosimano, M. P., Sepeda, N. D., Johnson, M. W., Finan, P. H., & Griffiths, R. R. (2021). Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA psychiatry, 78(5), 481–489. https://doi.org/10.1001/jamapsychiatry.2020.3285
12. Gukasyan, N., Davis, A. K., Barrett, F. S., Cosimano, M. P., Sepeda, N. D., Johnson, M. W., & Griffiths, R. R. (2022). Efficacy and safety of psilocybin-assisted treatment for major depressive disorder: Prospective 12-month follow-up. Journal of psychopharmacology (Oxford, England), 36(2), 151–158. https://doi.org/10.1177/02698811211073759
13. von Rotz, R., Schindowski, E. M., Jungwirth, J., Schuldt, A., Rieser, N. M., Zahoranszky, K., Seifritz, E., Nowak, A., Nowak, P., Jäncke, L., Preller, K. H., & Vollenweider, F. X. (2022). Single-dose psilocybin-assisted therapy in major depressive disorder: A placebo-controlled, double-blind, randomised clinical trial. EClinicalMedicine, 56, 101809. https://doi.org/10.1016/j.eclinm.2022.101809
14. Carhart-Harris, R., Giribaldi, B., Watts, R., Baker-Jones, M., Murphy-Beiner, A., Murphy, R., Martell, J., Blemings, A., Erritzoe, D., & Nutt, D. J. (2021). Trial of Psilocybin versus Escitalopram for Depression. The New England journal of medicine, 384(15), 1402–1411. https://doi.org/10.1056/NEJMoa2032994
15. Griffiths, R. R., Johnson, M. W., Carducci, M. A., Umbricht, A., Richards, W. A., Richards, B. D., Cosimano, M. P., & Klinedinst, M. A. (2016). Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: A randomized double-blind trial. Journal of psychopharmacology (Oxford, England), 30(12), 1181–1197. https://doi.org/10.1177/0269881116675513
16. Ross, S., Bossis, A., Guss, J., Agin-Liebes, G., Malone, T., Cohen, B., Mennenga, S. E., Belser, A., Kalliontzi, K., Babb, J., Su, Z., Corby, P., & Schmidt, B. L. (2016). Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. Journal of psychopharmacology (Oxford, England), 30(12), 1165–1180. https://doi.org/10.1177/0269881116675512
17. Goodwin, G. M., Aaronson, S. T., Alvarez, O., Arden, P. C., Baker, A., Bennett, J. C., Bird, C., Blom, R. E., Brennan, C., Brusch, D., Burke, L., Campbell-Coker, K., Carhart-Harris, R., Cattell, J., Daniel, A., DeBattista, C., Dunlop, B. W., Eisen, K., Feifel, D., Forbes, M., … Malievskaia, E. (2022). Single-Dose Psilocybin for a Treatment-Resistant Episode of Major Depression. The New England journal of medicine, 387(18), 1637–1648. https://doi.org/10.1056/NEJMoa2206443
18. Goodwin, G. M., Aaronson, S. T., Alvarez, O., Atli, M., Bennett, J. C., Croal, M., DeBattista, C., Dunlop, B. W., Feifel, D., Hellerstein, D. J., Husain, M. I., Kelly, J. R., Lennard-Jones, M. R., Licht, R. W., Marwood, L., Mistry, S., Páleníček, T., Redjep, O., Repantis, D., Schoevers, R. A., … Malievskaia, E. (2023). Single-dose psilocybin for a treatment-resistant episode of major depression: Impact on patient-reported depression severity, anxiety, function, and quality of life. Journal of affective disorders, 327, 120–127. https://doi.org/10.1016/j.jad.2023.01.108
19. Carhart-Harris, R. L., Bolstridge, M., Rucker, J., Day, C. M., Erritzoe, D., Kaelen, M., Bloomfield, M., Rickard, J. A., Forbes, B., Feilding, A., Taylor, D., Pilling, S., Curran, V. H., & Nutt, D. J. (2016). Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. The lancet. Psychiatry, 3(7), 619–627. https://doi.org/10.1016/S2215-0366(16)30065-7
20. Nayak, S. M., Jackson, H., Sepeda, N. D., Mathai, D. S., So, S., Yaffe, A., Zaki, H., Brasher, T. J., Lowe, M. X., Jolly, D. R. P., Barrett, F. S., Griffiths, R. R., Strickland, J. C., Johnson, M. W., Jackson, H., & Garcia-Romeu, A. (2023). Naturalistic psilocybin use is associated with persisting improvements in mental health and wellbeing: results from a prospective, longitudinal survey. Frontiers in psychiatry, 14, 1199642. https://doi.org/10.3389/fpsyt.2023.1199642
21. Evans, J., Robinson, O. C., Argyri, E. K., Suseelan, S., Murphy-Beiner, A., McAlpine, R., Luke, D., Michelle, K., & Prideaux, E. (2023). Extended difficulties following the use of psychedelic drugs: A mixed methods study. PloS one, 18(10), e0293349. https://doi.org/10.1371/journal.pone.0293349
22. Krebs, T. S., & Johansen, P. Ø. (2013). Psychedelics and mental health: a population study. PloS one, 8(8), e63972. https://doi.org/10.1371/journal.pone.0063972
23. Johansen, P. Ø., & Krebs, T. S. (2015). Psychedelics not linked to mental health problems or suicidal behavior: a population study. Journal of psychopharmacology (Oxford, England), 29(3), 270–279. https://doi.org/10.1177/0269881114568039
24. Hendricks, P. S., Thorne, C. B., Clark, C. B., Coombs, D. W., & Johnson, M. W. (2015). Classic psychedelic use is associated with reduced psychological distress and suicidality in the United States adult population. Journal of psychopharmacology (Oxford, England), 29(3), 280–288. https://doi.org/10.1177/0269881114565653
25. Halberstadt A. L. (2015). Recent advances in the neuropsychopharmacology of serotonergic hallucinogens. Behavioural brain research, 277, 99–120. https://doi.org/10.1016/j.bbr.2014.07.016
26. Mason, N. L., Kuypers, K. P. C., Müller, F., Reckweg, J., Tse, D. H. Y., Toennes, S. W., Hutten, N. R. P. W., Jansen, J. F. A., Stiers, P., Feilding, A., & Ramaekers, J. G. (2020). Me, myself, bye: regional alterations in glutamate and the experience of ego dissolution with psilocybin. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 45(12), 2003–2011. https://doi.org/10.1038/s41386-020-0718-8
27. Wojtas, A., Bysiek, A., Wawrzczak-Bargiela, A., Szych, Z., Majcher-Maślanka, I., Herian, M., Maćkowiak, M., & Gołembiowska, K. (2022). Effect of Psilocybin and Ketamine on Brain Neurotransmitters, Glutamate Receptors, DNA and Rat Behavior. International journal of molecular sciences, 23(12), 6713. https://doi.org/10.3390/ijms23126713
28. Lee, H. J., Tsang, V. W., Chai, B. S., Lin, M. C., Howard, A., Uy, C., & Elefante, J. O. (2023). Psilocybin's Potential Mechanisms in the Treatment of Depression: A Systematic Review. Journal of psychoactive drugs, 1–15. Advance online publication. https://doi.org/10.1080/02791072.2023.2223195
29. Hamilton, J. P., Furman, D. J., Chang, C., Thomason, M. E., Dennis, E., & Gotlib, I. H. (2011). Default-mode and task-positive network activity in major depressive disorder: implications for adaptive and maladaptive rumination. Biological psychiatry, 70(4), 327–333. https://doi.org/10.1016/j.biopsych.2011.02.003
30. Daws, R. E., Timmermann, C., Giribaldi, B., Sexton, J. D., Wall, M. B., Erritzoe, D., Roseman, L., Nutt, D., & Carhart-Harris, R. (2022). Increased global integration in the brain after psilocybin therapy for depression. Nature medicine, 28(4), 844–851. https://doi.org/10.1038/s41591-022-01744-z
31. Lydon-Staley, D. M., Kuehner, C., Zamoscik, V., Huffziger, S., Kirsch, P., & Bassett, D. S. (2019). Repetitive negative thinking in daily life and functional connectivity among default mode, fronto-parietal, and salience networks. Translational psychiatry, 9(1), 234. https://doi.org/10.1038/s41398-019-0560-0
32. Mertens, L. J., Wall, M. B., Roseman, L., Demetriou, L., Nutt, D. J., & Carhart-Harris, R. L. (2020). Therapeutic mechanisms of psilocybin: Changes in amygdala and prefrontal functional connectivity during emotional processing after psilocybin for treatment-resistant depression. Journal of psychopharmacology (Oxford, England), 34(2), 167–180. https://doi.org/10.1177/0269881119895520
33. Sloshower, J., Zeifman, R. J., Guss, J., Krause, R., Safi-Aghdam, H., Pathania, S., Pittman, B., & D'Souza, D. C. (2024). Psychological flexibility as a mechanism of change in psilocybin-assisted therapy for major depression: results from an exploratory placebo-controlled trial. Scientific reports, 14(1), 8833. https://doi.org/10.1038/s41598-024-58318-x
34. Davis, A. K., Barrett, F. S., & Griffiths, R. R. (2020). Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. Journal of contextual behavioral science, 15, 39–45. https://doi.org/10.1016/j.jcbs.2019.11.004
35. Doss, M. K., Považan, M., Rosenberg, M. D., Sepeda, N. D., Davis, A. K., Finan, P. H., Smith, G. S., Pekar, J. J., Barker, P. B., Griffiths, R. R., & Barrett, F. S. (2021). Psilocybin therapy increases cognitive and neural flexibility in patients with major depressive disorder. Translational psychiatry, 11(1), 574. https://doi.org/10.1038/s41398-021-01706-y
36. Barba, T., Buehler, S., Kettner, H., Radu, C., Cunha, B. G., Nutt, D. J., Erritzoe, D., Roseman, L., & Carhart-Harris, R. (2022). Effects of psilocybin versus escitalopram on rumination and thought suppression in depression. BJPsych open, 8(5), e163. https://doi.org/10.1192/bjo.2022.565
37. Watts, R., Day, C., Krzanowski, J., Nutt, D., & Carhart-Harris, R. (2017). Patients’ accounts of increased “connectedness” and “acceptance” after psilocybin for treatment-resistant depression. Journal of Humanistic Psychology, 57(5), 520-564.
38. Roseman, L., Nutt, D. J., & Carhart-Harris, R. L. (2018). Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression. Frontiers in pharmacology, 8, 974. https://doi.org/10.3389/fphar.2017.00974
39. Romeo, B., Hermand, M., Pétillion, A., Karila, L., & Benyamina, A. (2021). Clinical and biological predictors of psychedelic response in the treatment of psychiatric and addictive disorders: A systematic review. Journal of psychiatric research, 137, 273–282. https://doi.org/10.1016/j.jpsychires.2021.03.002
40. Levin, A. W., Lancelotta, R., Sepeda, N. D., Gukasyan, N., Nayak, S., Wagener, T. L., Barrett, F. S., Griffiths, R. R., & Davis, A. K. (2024). The therapeutic alliance between study participants and intervention facilitators is associated with acute effects and clinical outcomes in a psilocybin-assisted therapy trial for major depressive disorder. PloS one, 19(3), e0300501. https://doi.org/10.1371/journal.pone.0300501
41. Murphy, R., Kettner, H., Zeifman, R., Giribaldi, B., Kartner, L., Martell, J., Read, T., Murphy-Beiner, A., Baker-Jones, M., Nutt, D., Erritzoe, D., Watts, R., & Carhart-Harris, R. (2022). Therapeutic Alliance and Rapport Modulate Responses to Psilocybin Assisted Therapy for Depression. Frontiers in pharmacology, 12, 788155. https://doi.org/10.3389/fphar.2021.788155
42. Goodwin, G. M., Price, J., De Bodinat, C., & Laredo, J. (2017). Emotional blunting with antidepressant treatments: A survey among depressed patients. Journal of affective disorders, 221, 31–35. https://doi.org/10.1016/j.jad.2017.05.048
43. Price, J., Cole, V., & Goodwin, G. M. (2009). Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. The British journal of psychiatry : the journal of mental science, 195(3), 211–217. https://doi.org/10.1192/bjp.bp.108.051110
44. Roseman, L., Demetriou, L., Wall, M. B., Nutt, D. J., & Carhart-Harris, R. L. (2018). Increased amygdala responses to emotional faces after psilocybin for treatment-resistant depression. Neuropharmacology, 142, 263–269. https://doi.org/10.1016/j.neuropharm.2017.12.041
45. Lindegaard T. (2023). Do Psychedelics Facilitate Emergence of Unconscious Psychological Processes?. Psychodynamic psychiatry, 51(3), 270–286. https://doi.org/10.1521/pdps.2023.51.3.270
46. Brennan, W., Kelman, A. R., & Belser, A. B. (2023). A systematic review of reporting practices in psychedelic clinical trials: Psychological support, therapy, and psychosocial interventions. Psychedelic Medicine, 1(4). https://doi.org/10.1089/psymed.2023.0007
47. Nichols D. E. (2016). Psychedelics. Pharmacological reviews, 68(2), 264–355. https://doi.org/10.1124/pr.115.011478
48. Johnson, M., Richards, W., & Griffiths, R. (2008). Human hallucinogen research: guidelines for safety. Journal of psychopharmacology (Oxford, England), 22(6), 603–620. https://doi.org/10.1177/0269881108093587
49. Johnson, M. W., Sewell, R. A., & Griffiths, R. R. (2012). Psilocybin dose-dependently causes delayed, transient headaches in healthy volunteers. Drug and alcohol dependence, 123(1-3), 132–140. https://doi.org/10.1016/j.drugalcdep.2011.10.029
50. Rootman, J. M., Kiraga, M., Kryskow, P., Harvey, K., Stamets, P., Santos-Brault, E., Kuypers, K. P. C., & Walsh, Z. (2022). Psilocybin microdosers demonstrate greater observed improvements in mood and mental health at one month relative to non-microdosing controls. Scientific reports, 12(1), 11091. https://doi.org/10.1038/s41598-022-14512-3
51. Kaertner, L. S., Steinborn, M. B., Kettner, H., Spriggs, M. J., Roseman, L., Buchborn, T., Balaet, M., Timmermann, C., Erritzoe, D., & Carhart-Harris, R. L. (2021). Positive expectations predict improved mental-health outcomes linked to psychedelic microdosing. Scientific reports, 11(1), 1941. https://doi.org/10.1038/s41598-021-81446-7
52. Polito, V., & Stevenson, R. J. (2019). A systematic study of microdosing psychedelics. PloS one, 14(2), e0211023. https://doi.org/10.1371/journal.pone.0211023
53. Lea, T., Amada, N., & Jungaberle, H. (2020). Psychedelic Microdosing: A Subreddit Analysis. Journal of psychoactive drugs, 52(2), 101–112. https://doi.org/10.1080/02791072.2019.1683260
54. Ryan, R. S., Copello, A., & Fox, A. P. (2023). Experiences of microdosing psychedelics in an attempt to support wellbeing and mental health. BMC psychiatry, 23(1), 160. https://doi.org/10.1186/s12888-023-04628-9
55. Johnstad P. G. (2018). Powerful substances in tiny amounts: An interview study of psychedelic microdosing. Nordisk alkohol- & narkotikatidskrift : NAT, 35(1), 39–51. https://doi.org/10.1177/1455072517753339
56. Cavanna, F., Muller, S., de la Fuente, L. A., Zamberlan, F., Palmucci, M., Janeckova, L., Kuchar, M., Pallavicini, C., & Tagliazucchi, E. (2022). Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study. Translational psychiatry, 12(1), 307. https://doi.org/10.1038/s41398-022-02039-0
57. Marschall, J., Fejer, G., Lempe, P., Prochazkova, L., Kuchar, M., Hajkova, K., & van Elk, M. (2022). Psilocybin microdosing does not affect emotion-related symptoms and processing: A preregistered field and lab-based study. Journal of psychopharmacology (Oxford, England), 36(1), 97–113. https://doi.org/10.1177/02698811211050556
58. Rouaud, A., Calder, A. E., & Hasler, G. (2024). Microdosing psychedelics and the risk of cardiac fibrosis and valvulopathy: Comparison to known cardiotoxins. Journal of psychopharmacology (Oxford, England), 38(3), 217–224. https://doi.org/10.1177/02698811231225609

.svg)









.svg)